Cranial procedures begin with access. Opening the skull introduces potential exposure to infection and external contaminants. The skin, bone, and meninges are all breached. Even under sterile conditions, bacteria may enter. Infections can develop at the surgical site or deeper. Meningitis, abscesses, or bone infections may follow. Preoperative antibiotics reduce microbial load beforehand. Strict sterile technique continues throughout the operation. Post-surgery monitoring includes temperature, labs, and wound condition.
Bleeding may occur within the brain tissue or surrounding spaces
Vascular disruption poses major concern. Bleeding may occur within the brain tissue or surrounding spaces. Small vessels can tear during dissection. Hematomas increase intracranial pressure quickly. Subdural or epidural bleeding can compress healthy brain areas. Surgeons control bleeding with cauterization or packing. Hemostasis is continuously checked before closure. Postoperative imaging identifies hidden bleeds. Urgent evacuation may be necessary if pressure rises.
Swelling from fluid shifts can elevate pressure inside the skull
Surgery changes brain fluid dynamics. Swelling from fluid shifts can elevate pressure inside the skull. The brain sits in a fixed bony case. Any increase in volume causes compression. Cerebral edema may arise hours after surgery. Neurological exams track subtle shifts in consciousness. Mannitol or steroids may reduce swelling. Drain placement helps relieve fluid buildup. Intracranial pressure monitors guide critical interventions.
Seizures may develop after disruption of cortical pathways
Electrical activity becomes unpredictable. Seizures may develop after disruption of cortical pathways. Tissue manipulation may irritate neurons. Scar tissue creates abnormal conduction circuits. Not all seizures appear as convulsions. Some cause brief lapses in awareness. Antiepileptic medications are often prescribed postoperatively. Risk varies based on surgery location. Seizure patterns may change during recovery.
Cognitive or speech difficulties may follow depending on surgical site
Function ties closely to anatomy. Cognitive or speech difficulties may follow depending on surgical site. Temporal and frontal lobes manage memory and language. Disruption may cause word-finding or processing delays. Some changes are temporary and improve with therapy. Others reflect permanent tissue damage. Neuropsychological tests baseline these abilities preoperatively. Rehabilitation targets specific deficits afterward.
Motor weakness or numbness may result from proximity to functional tissue
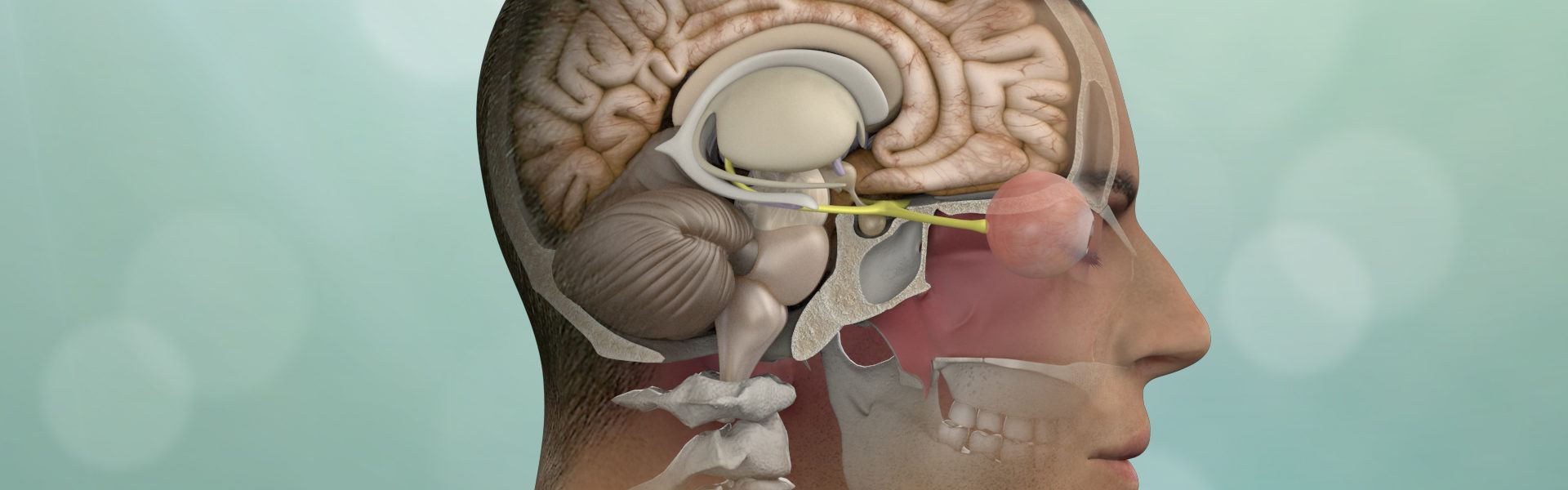
Movement centers lie in delicate zones. Motor weakness or numbness may result from proximity to functional tissue. The primary motor cortex controls voluntary movement. Even slight disturbance affects coordination. Swelling or retraction pressure can contribute. Nerves may also be disturbed during access. Physical therapy often starts quickly after surgery. Motor mapping during surgery reduces unintentional injury.
Stroke may occur if blood flow is interrupted or reduced during surgery
Circulatory stability is crucial. Stroke may occur if blood flow is interrupted or reduced during surgery. Clots, vasospasm, or mechanical blockage can reduce oxygen delivery. Affected areas suffer from infarction or tissue death. Real-time monitoring tracks perfusion changes. Surgical positioning minimizes vessel compression. Blood thinners or antiplatelets are sometimes used. Stroke risk depends on age, health, and duration.
CSF leaks through the surgical opening may lead to complications
Brain fluid containment matters. CSF leaks through the surgical opening may lead to complications. Cerebrospinal fluid cushions and protects neural tissue. Dural tears can result in fluid escaping. Symptoms include headache, nausea, or clear drainage. Persistent leaks increase meningitis risk. Surgical repair or lumbar drains may be required. Early recognition avoids escalation.
Anesthesia poses separate risks involving cardiovascular and respiratory systems
Support systems face their own strain. Anesthesia poses separate risks involving cardiovascular and respiratory systems. Blood pressure may drop suddenly under sedation. Airway management must remain stable during positioning. Heart rhythm disturbances may arise. Older patients with comorbidities are especially vulnerable. Anesthesiologists adjust medications based on real-time changes. Recovery from anesthesia is carefully timed with surgical closure.
Emotional and behavioral changes may emerge after recovery begins
Personality shifts sometimes follow. Emotional and behavioral changes may emerge after recovery begins. Brain regions control mood, impulse, and behavior. Swelling, scarring, or reconnection may affect these areas. Depression, irritability, or disinhibition can appear. Family may notice changes before the patient does. Psychological support becomes part of the recovery plan. Medications or counseling assist with adjustment.
