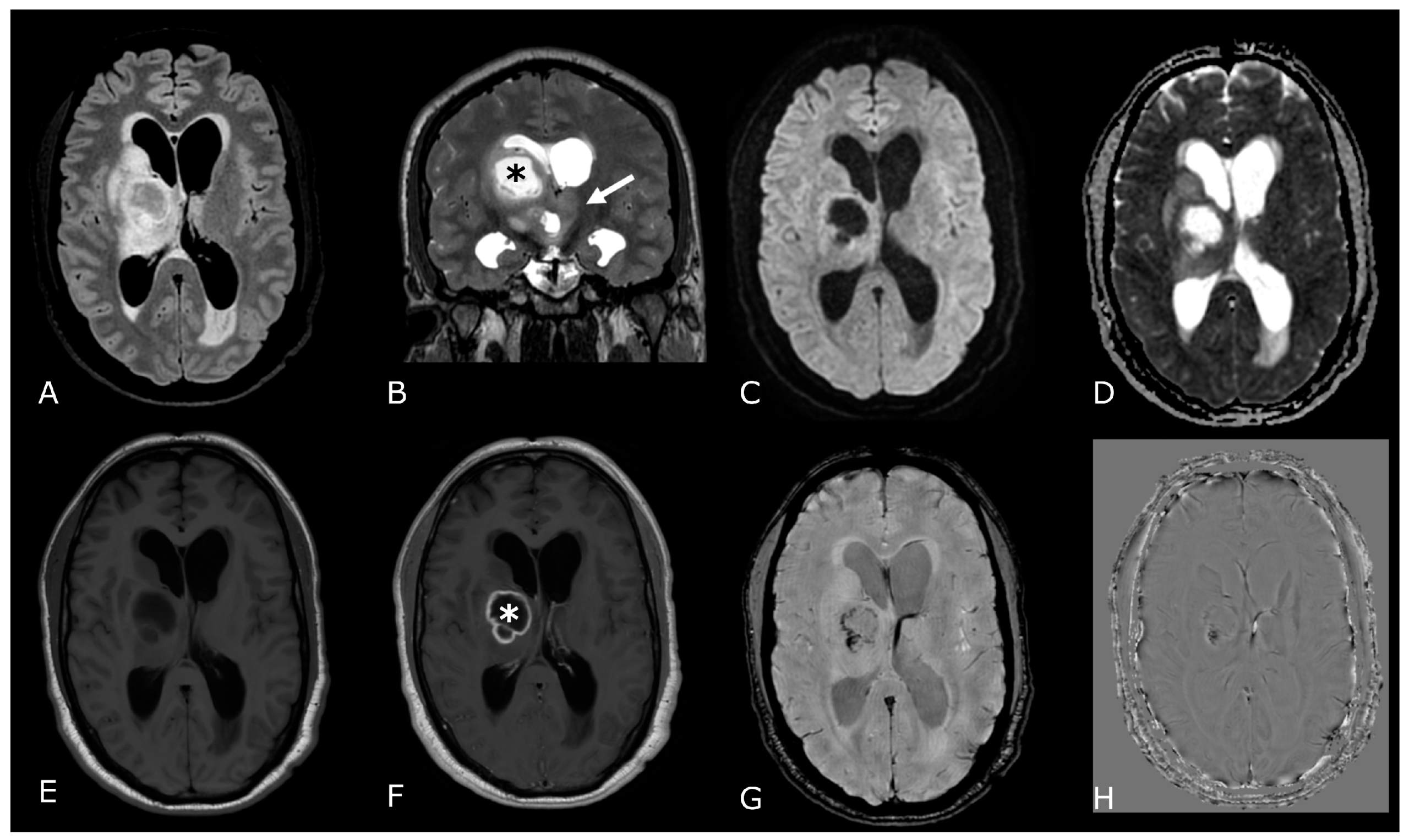
Preoperative imaging forms the foundation. Magnetic resonance imaging captures detailed soft tissue contrasts within the brain. Unlike CT scans, MRI doesn’t rely on radiation. Instead, it uses magnetic fields and radiofrequency. This distinction allows clearer mapping of delicate brain structures. Surgeons rely on these details for accurate spatial understanding. Each scan offers slices from multiple directions. Tumors, lesions, and cysts are better differentiated. MRI shows edema, blood flow, and mass effect precisely.
Functional MRI identifies regions responsible for language, memory, and movement
Planning requires more than structure. Functional MRI identifies regions responsible for language, memory, and movement. These scans detect oxygen changes linked to brain activity. During tasks, active regions show different signal intensity. The result is a functional overlay on anatomical maps. Neurosurgeons use this to avoid eloquent areas. Each brain varies slightly, so mapping is individualized. This reduces cognitive and motor risks post-surgery.
Diffusion tensor imaging visualizes white matter tracts connecting various brain regions
Pathways require separate imaging. Diffusion tensor imaging visualizes white matter tracts connecting various brain regions. Water movement follows fiber orientation. Tractography reconstructs directional pathways graphically. This reveals how nearby tumors distort or displace these tracts. Resection near vital fibers increases risk of paralysis or speech loss. Planning involves deciding where incisions preserve maximal connectivity. These maps evolve alongside tumor growth or edema changes.
MR angiography displays arterial and venous anatomy without the need for contrast dye
Vascular layout must be included. MR angiography displays arterial and venous anatomy without the need for contrast dye. This becomes vital when operating near the Circle of Willis. Aneurysms, arteriovenous malformations, and stenosis appear clearly. Flow patterns guide clamping or bypass techniques. Venous drainage routes also matter during access. Disrupting these structures risks catastrophic bleeding. Surgeons review vascular models before incision.
MRI helps distinguish between active tumor tissue and post-treatment scarring
Tissue characterization aids in interpretation. MRI helps distinguish between active tumor tissue and post-treatment scarring. Gadolinium contrast enhances tumor borders distinctly. Areas of necrosis or fibrosis show different signal profiles. Radiation effects can resemble recurrence. Advanced sequences like perfusion-weighted imaging clarify uncertain zones. Planning must include what’s viable and what’s reactive. This avoids unnecessary tissue removal.
Real-time MRI during surgery allows intraoperative adjustments to the surgical plan
Technology continues into the operating room. Real-time MRI during surgery allows intraoperative adjustments to the surgical plan. The brain can shift once opened—known as brain shift. Initial landmarks may no longer align. Intraoperative scans confirm tumor boundaries after partial resection. If unexpected tissue remains, surgeons adjust accordingly. This reduces incomplete resection and avoids overcutting. The suite includes specialized MRI-compatible tools.
MRI contributes to trajectory planning for minimally invasive interventions
Even access paths are pre-imaged. MRI contributes to trajectory planning for minimally invasive interventions. Biopsies or electrode placements demand high spatial accuracy. Deep structures like thalamus or brainstem require safe navigation. MRI scans determine angle, depth, and target zone. Frameless stereotactic systems register patient anatomy. Errors of even a few millimeters matter. Combining scans with navigation improves accuracy.
Lesions in eloquent areas require conservative approaches informed by precise MRI data
Location determines surgical strategy. Lesions in eloquent areas require conservative approaches informed by precise MRI data. Aggressive resections risk permanent deficits. Smaller incisions may preserve speech or movement. Sometimes, only partial resection is recommended. MRI helps define acceptable boundaries. These judgments require weighing function over volume. Postoperative recovery often depends on these early decisions.
MRI monitors postoperative changes and checks for recurrence over time
Follow-up uses the same modality. MRI monitors postoperative changes and checks for recurrence over time. Scar tissue and residual tumor evolve differently. Interval scanning shows whether enhancement grows. Comparing scans across months reveals treatment response. Surgeons also assess swelling, cavity changes, or new lesions. Timing varies by diagnosis and intervention type. MRI guides decisions for additional therapy or observation.
Combining MRI data with clinical judgment creates safer and more personalized surgical outcomes
No scan replaces human decision-making. Combining MRI data with clinical judgment creates safer and more personalized surgical outcomes. Imaging complements but doesn’t dictate choices. Surgeons match visuals with symptoms, history, and goals. MRI may show incidental findings not linked to disease. Context refines how those findings are interpreted. Communication between radiologist and surgeon remains critical.
