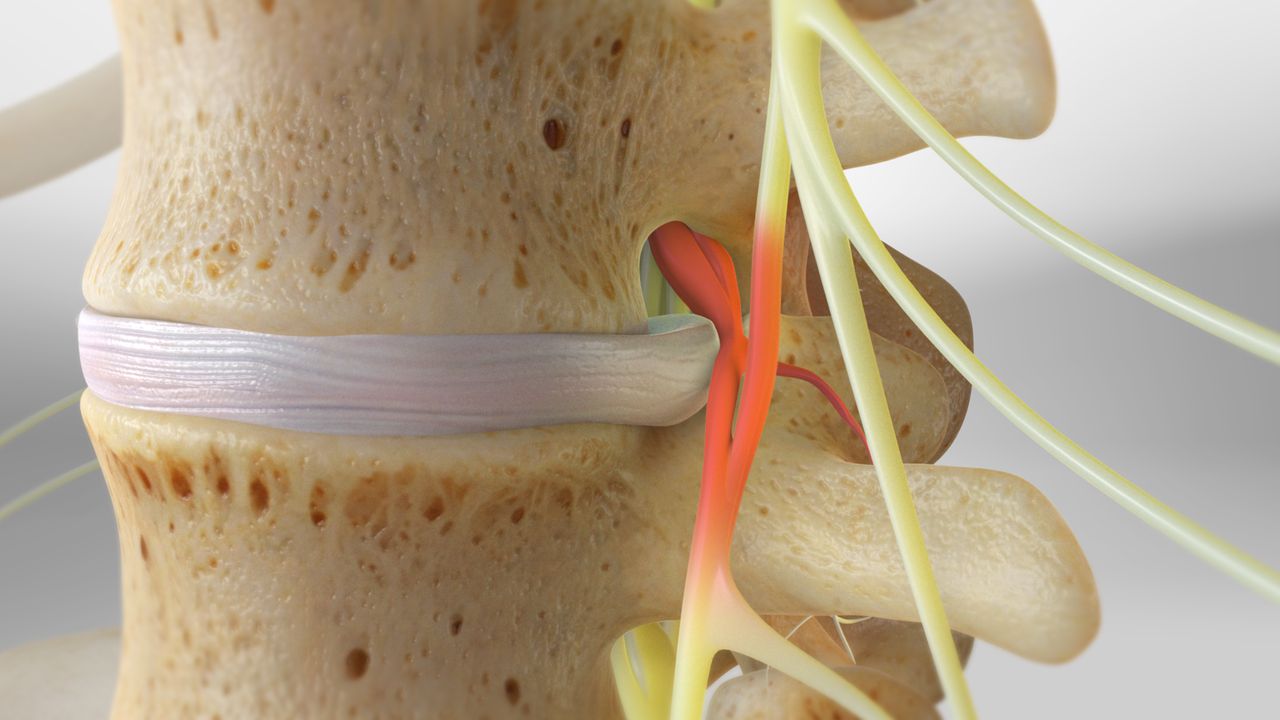
A herniated disc occurs when the soft center of a spinal disc pushes through its outer layer. The spine is made up of bones called vertebrae separated by spongy discs. These discs act as cushions and allow flexibility during movement. When a disc’s outer shell weakens or tears, the inner material bulges outward. This bulge can press on nearby nerves, causing pain or numbness. Herniation is most common in the lower back or neck. Heavy lifting, trauma, or age-related wear can trigger the condition. Sometimes it happens suddenly, sometimes gradually. Symptoms vary depending on disc location and nerve involvement.
Symptoms may include back pain, leg weakness, tingling, or numbness depending on the affected nerve
Symptoms may include back pain, leg weakness, tingling, or numbness depending on the affected nerve. If the herniated disc presses on the sciatic nerve, symptoms may radiate down the leg. This is called sciatica and often worsens with movement or coughing. Neck disc herniation can cause arm pain or hand weakness. Pain may be sharp or dull, constant or intermittent. Nerve compression often leads to burning sensations or muscle fatigue. In severe cases, bowel or bladder control may be affected. These signs indicate a need for urgent medical attention. Not all herniated discs cause pain, but many require evaluation.
Diagnosis relies on physical exams, symptom history, and imaging tests like MRI or CT scans
Diagnosis relies on physical exams, symptom history, and imaging tests like MRI or CT scans. Doctors assess reflexes, strength, and sensation to determine which nerves are involved. The straight leg raise test helps identify nerve root irritation in the leg. MRI provides detailed images of soft tissues and disc structure. CT scans show bone alignment and may reveal fractures or narrowing. X-rays rule out other spinal conditions but don’t show herniation directly. Sometimes, contrast dye is used to improve visibility of nerve compression. Proper diagnosis is essential before selecting a treatment path.
Many herniated discs improve without surgery through rest, activity modification, and targeted physical therapy
Many herniated discs improve without surgery through rest, activity modification, and targeted physical therapy. Pain often decreases within weeks of conservative care. Patients are advised to avoid heavy lifting and prolonged sitting. Gentle movement and walking may help reduce pressure on the disc. Physical therapy includes stretching, strengthening, and posture correction exercises. Therapists teach body mechanics to prevent reinjury. Ice and heat therapy can ease pain between sessions. Medications may be used to control discomfort during recovery. These include anti-inflammatories and muscle relaxants. Most patients recover without invasive treatment if guidance is followed consistently.
Over-the-counter or prescription medications can reduce inflammation, muscle spasms, and nerve-related discomfort
Over-the-counter or prescription medications can reduce inflammation, muscle spasms, and nerve-related discomfort. Nonsteroidal anti-inflammatory drugs help control swelling around the nerve root. Muscle relaxants may ease spasms triggered by nerve irritation. Oral steroids can reduce inflammation more aggressively in some cases. Neuropathic pain medications target nerve sensitivity and burning sensations. Stronger options like opioids are used briefly if other methods fail. Medication plans are tailored to symptom type and severity. Doctors monitor side effects and adjust dosages as needed. Long-term relief usually depends on combining medications with physical therapy and lifestyle changes.
Epidural steroid injections may be used to deliver anti-inflammatory medication directly around irritated spinal nerves
Epidural steroid injections may be used to deliver anti-inflammatory medication directly around irritated spinal nerves. These injections reduce swelling and provide pain relief in targeted areas. The procedure is usually done under X-ray guidance in a clinical setting. Relief may begin within days and last weeks or months. Patients typically receive a series of injections rather than just one. These are used when pain limits function or therapy progress. Injections are not a cure but part of a broader plan. Risks include infection, bleeding, or temporary numbness. Effectiveness varies by individual and location of herniation.
Surgery is considered when conservative treatment fails or when weakness and nerve compression worsen
Surgery is considered when conservative treatment fails or when weakness and nerve compression worsen. Persistent pain lasting longer than six weeks despite therapy may require surgical review. Loss of bladder or bowel control demands immediate surgical evaluation. The most common procedure is discectomy, which removes the herniated portion of the disc. Minimally invasive techniques shorten recovery and reduce tissue damage. Some cases require spinal fusion to stabilize the area after disc removal. Surgical risks include infection, bleeding, or recurrence. Outcomes are generally good when procedures are done for the right reasons. Not everyone with a herniated disc needs surgery.
Recovery from surgery usually includes restricted activity, gradual rehabilitation, and long-term posture improvement
Recovery from surgery usually includes restricted activity, gradual rehabilitation, and long-term posture improvement. Patients often begin walking soon after the procedure. Heavy lifting and twisting are avoided for several weeks. Physical therapy starts shortly after to rebuild strength and flexibility. Therapists guide safe movements and prevent overexertion during healing. Full recovery may take weeks to months depending on individual condition. Long-term prevention focuses on ergonomic habits and spine health. Patients learn to lift safely and avoid prolonged poor posture. Lifestyle changes matter as much as the surgery itself. Recurrence is less likely with continued attention to mechanics.
Prevention focuses on spine support, body mechanics, and reducing stress on discs during everyday activities
Prevention focuses on spine support, body mechanics, and reducing stress on discs during everyday activities. Regular exercise strengthens core muscles that stabilize the spine. Stretching maintains flexibility and reduces strain during bending or lifting. Proper posture minimizes uneven disc pressure while sitting or standing. Lifting with legs—not the back—protects spinal discs. Breaks during long sitting or driving reduce cumulative stress. Maintaining a healthy weight lessens spinal load. Smoking cessation is also advised as nicotine affects disc nutrition. Small daily adjustments help avoid future herniation episodes. Prevention requires consistency, not intensity.
